PART 3: Evidence of reckless practice of medicine
(All materials presented in this section are taken directly from the evidences produced in the “criminal” and “civil” appeals pending before the Supreme Court)
Anuradha died from an act of gross medical negligence. Despite regular incidence of “medical negligence” in hospitals and nursing homes across India, legal prosecution of the errant doctors and hospitals was virtually non-existent in India when Anuradha became a victim of reckless medical malpractice during a social visit to India in 1998. Being a physician born and raised in India, Kunal was well aware about the seemingly impossible task of bring the doctors who were responsible for the untimely demise of his beloved wife to justice. All of Kunal’s close doctor friends in India were also of the opinion that despite an absolute brazen act of medical negligence that took Anuradha’s life, there is no chance to bring justice for these “top” doctors responsible for Anuradha’s death. Although Anuradha was an India-born naturalized US citizen, the case for medical negligence had to be fought and won at the scene of the alleged crime – the City of Joy where this angelic love story between Kunal and Anuradha started almost 13 years earlier. Even though legal provision for “criminal prosecution” of a doctor causing death of a patient through reckless treatment (“manslaughter”) exists in the Indian Penal Code (IPC) for almost 150 years (under IPC Section 304A), not a single registered, allopathic doctor has ever been convicted under this law in the history of Indian medico-legal jurisprudence until 1998. Although not very common, many doctors in the UK and USA have been convicted for “criminal negligence” and spent time in jail for causing death of a patient through reckless therapy. Returning to their dream house in Columbus, all alone in a devastated condition, Kunal started his journey for this almost impossible “crusade” to bring justice not only for his departed wife but also for the countless innocent victims of medical negligence in India. Kunal started this “crusade” for justice against the negligent doctors in Calcutta by contacting the very top medical experts in different countries in the relevant fields (dermatology and pharmacology) for their opinions about Anuradha's treatment because opinions from medical experts play a crucial role for establishing a case of “medical negligence”.
The reckless therapy that eventually killed Anuradha started with Dr. Sukumar Mukherjee who first treated Anuradha in his chamber at Nightingale Diagnostic Center in Calcutta in the evening of 7th May, 1998 when Anuradha had severe skin rashes and some fever. Dr. Mukherjee immediately injected her with 80 mg of “Depomedrol” and advised that she must continue the “Depomedrol” injection at 80 mg BID (twice daily) for at least the next three days. Dr. Mukherjee’s hand-written prescription is shown in the next page. He diagnosed Anuradha’s condition as “Angioneurotic oedema with allergic vasculitis” and also prescribed some other medicines. This was the beginning of a therapy unheard of in the annals of medical science that eventually snatched the life of young woman. As discussed previously, “Depomedrol” is used as a steroid therapy only in some “chronic” clinical conditions like “asthma” and “arthritis” because of its “long-acting” role. Patients with “chronic” conditions do not have to take steroid everyday since one injection of “Depomedrol” lasts in the body for up to one month.
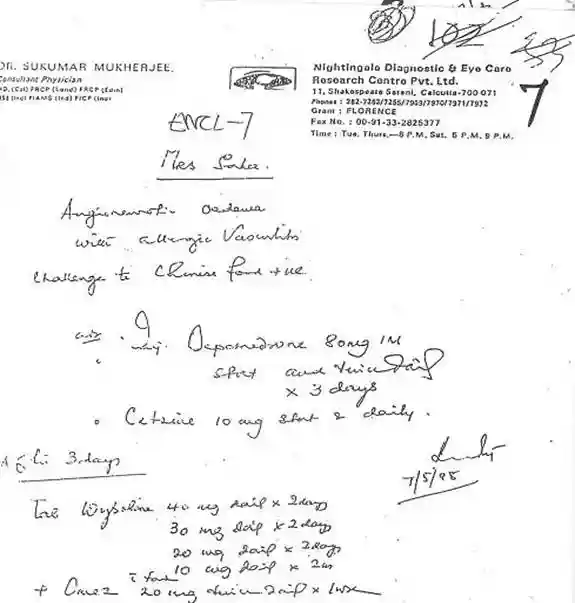
For “acute” clinical conditions where steroids are recommended, only “quick-acting” steroids like “Decadron” or “Solumedrol” are used for its fast action and quick elimination from the body. This is why “quick-acting”, and not the “long-acting, steroids can be repeated daily or even several times a day. Frequent injections of long-acting steroids like “Depomedrol” would cause a devastating adverse effect (“suppression of natural immunity”) in the body by accumulation of the drug to a very high level. So why did Dr. Mukherjee choose to use “Depomedrol” as a steroid to treat Anuradha on 7th May, 1998 when she came with an “acute” skin condition? Dr. Mukherjee could not answer this question when he was asked during his examination in the court.
But even more shocking than Dr. Mukherjee’s choice of “Depomedrol” was his selection of its astronomically high “dose”. He injected Anuradha with 80 mg “Depomedrol” straight away in his chamber (“stat”; as written in his prescription) in the evening of 7th May, 1998 and asked her to continue the same injection at 80 mg twice daily for the next three days. The maximum recommended dose of “Depomedrol” for any clinical condition is 40-120 mg at least 1-2 weeks or longer intervals. On Dr. Mukherjee’s advice, “Depomedrol” was injected to Anuradha 160 mg everyday (80 mg twice daily) for the next 7 days (Dr. Mukherjee repeated the same prescription after Anuradha on 11th May, 1998 at after Anuradha was admitted at AMRI hospital, see his second prescription in the next page). So, Anuradha basically received a dangerous steroid preparation (“Depomedrol”) at 20-50 times its maximum recommended dose as prescribed by Dr. Mukherjee. As shown below, a plethora of other documentary evidences including written experts’ opinions and direct testimonies were presented in this case to establish the brazenly wrongful and reckless use of “Depomedrol” by Dr. Mukherjee. On the contrary, not a single expert’s opinion, either as a written statement or as a witness in the court was produced in this case by any of the accused doctors suggesting that “Depomedrol” at 80 mg twice daily as Dr. Mukherjee prescribed could be given to any patient under any clinical condition. A brief summary of the evidence showing reckless use of far too excessive “Depomedrol” by Dr. Mukherjee is presented below. This is not an exhaustive list of evidence that were produced by the prosecution in this matter but only some of the irrefutable proofs are shown below.
Evidence of reckless use of “Depomedrol”:
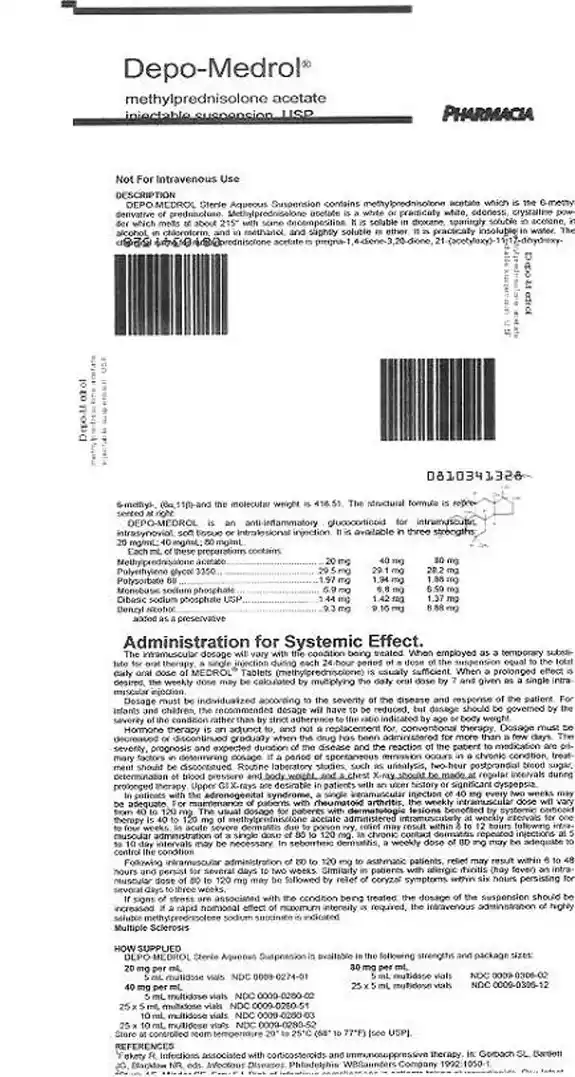
1. “Package Insert” of Depomedrol:
The ultimate authority as to how much of any drug (“dosage”) should be used in any medical condition is decided by the manufacturer of the particular drug after adequate basic and clinical studies. The Food and Drug Administration (FDA) ultimately makes the final decision for approval of any drug to be used on patients based on these pre-clinical and clinical studies by the manufacturer. Thus, the use and dose of any medicine as given by the manufacturer in the “package insert” of each product is the final authority for its use which doctors must adhere to for use their patients. The “package insert” of “Depomedrol” as produced by the manufacturer of the drug, Pharmacia (same as “Pharmacia Upjohn”) was submitted in the court (a copy of the “package insert” of Depomedrol is shown on page 18). As seen in the “package insert” (under “Administration for Systemic Effect”), “Depomedrol” is not even recommended either for “TEN” (the disease Anuradha had) or “Angioneurotic oedema” (the wrong diagnosis made by Dr. Mukherjee). About “Depomedrol” dose for any skin condition (which Anuradha obviously had), the “package insert” categorically says that the dose of “Depomedrol” for use in any dermatologic condition is “40-120 mg” given at “weekly intervals for 1-4 weeks”. In fact, as this “package insert” shows beyond the shadow of any doubt, for any disease, not just in dermatologic conditions, “Depomedrol” can only be given maximum at 120 mg at an interval of at least 1 week.
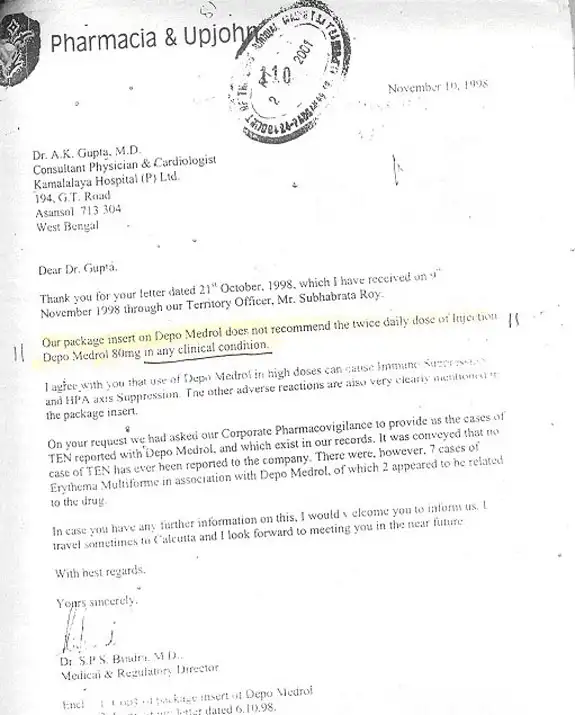
2. Opinion by Indian manufacturer of “Depomedrol”:
Pharmacia is a US-based drug company. “Depomedrol” is circulated in India by the Indian branch of Pharmacia company. They were contacted for their opinion about the use of Depomedrol at “80 mg twice daily” dose as prescribed by Dr. Mukherjee. The Medical and Regulatory Director of Pharmacia in India, Dr. S.P. Bindra submitted a written response in which he has categorically stated, “Package insert of Depomedrol does not recommend the twice daily dose of injection Depomedrol 80 mg in any clinical condition”. Dr. Bindra further stated that this excessive dose of “Depomedrol” (80 mg twice daily) can obviously cause immunosuppression in any patient (see Dr. Bindra’s letter on page 20). During the “criminal trial” in Calcutta, medical manager of Pharmacia, Dr. A. Shinde was summoned and he also directly testified the very same facts about “Depomedrol”.
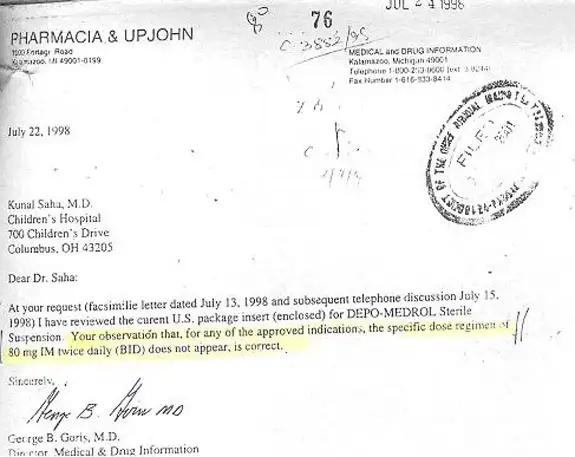
3. Opinion from US manufacture of “Depomedrol”:
The original Pharmacia company in Kalamazoo, Michigan, USA was also contacted for their opinion about the “80 mg twice daily” dose of “Depomedrol”. In a written statement sent to Anuradha’s husband which has been filed in the court, they have also corroborated that “Depomedrol” cannot be given at 80 mg twice daily dose for any clinical condition (see the letter from the Medical Director of the US Pharmacia Upjohn on page 21).
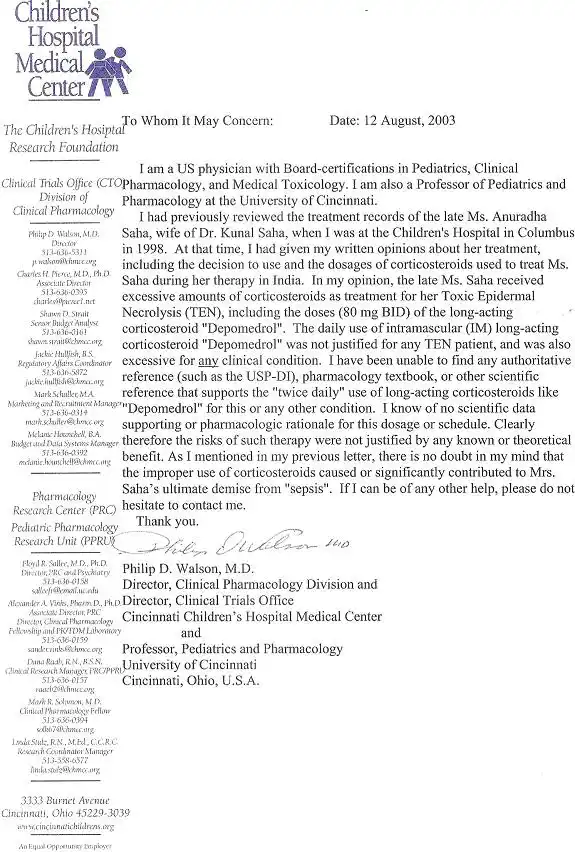
4. Opinion from world-renowned Pharmacology experts:
Dr. Philip Walson is a world-renowned clinical pharmacologist and associate editor of the United States Pharmacopiea- Drug Index (USP-DI), most commonly used drug index book by world-wide doctors. Dr. Walson has evaluated the treatment given to Anuradha with 80 mg twice daily dose of “Depomedrol”. His written opinion has been filed in the court in which Dr. Walson has categorically stated, “In my opinion, the late Mrs. Saha received excessive amount of corticosteroid for her TEN, including the dose (80 mg BID) of long-acting corticosteroid “Depomedrol”. The daily use of intramascular long-acting corticosteroid “Depomedrol” was not justified for any TEN patient and was also excessive for any clinical condition……………there is no doubt in my mind that the improper use of corticosteroid caused or significantly contributed to Mrs. Saha’s ultimate death from “sepsis”.” (see Dr. Walson’s letter on page 22). Another highly respected Pharmacology expert from India, Prof. Salil Bhattacharya of Benaras Hindu University, directly testified in the “criminal trial” in Calcutta and given the exact same opinion about “Depomedrol” as Dr. Walson.
5. Opinion from India’s top expert in Dermatology:
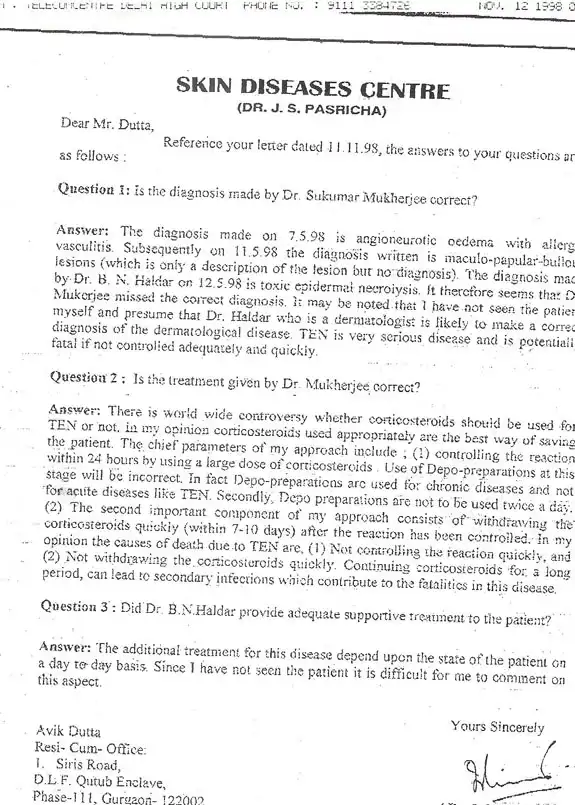
Dr. J.S. Pasricha is the ex-head of the department of Dermatology at the All India Institute of Medical Sciences (AIIMS) and probably the most well-known Indian dermatologist today. Dr. Pasricha has also examined treatment of Anuradha and provided written answers to questions asked by Kunal’s attorney. When asked, “Is the treatment given by Dr. Mukherjee correct?”, Dr. Pasricha answered, “……The chief parameters of my approach include, 1) controlling the reaction within 24 hours by using a large dose of corticosteroid. Use of Depo-preparations (“Depomedrol”) at this stage will be incorrect. In fact, Depo-preparations (“Depomedrol”) are used for chronic diseases and not for acute diseases like TEN. Secondly, Depo-preparations are not to be used twice a day” (see on page 23).
Apart from these evidences discussed above, many other medical experts produced by the prosecution either as a witness in the “criminal trial” or through written submissions including Dr. Anil Gupta, Dr. Anil Shinde, Dr. Salil Bhattacharya, Dr. Kunal Saha, Dr. Peter Fritsch (Austria), Dr. David Fine (USA), Dr. Gerald Pierard (Belgium), and Dr. J.C. Roujeau (France) have all testified about the wrongful use of “Depomedrol”. In contrast, the accused doctors have failed to produce even a single MBBS doctor to testify on their behalf that “Depomedrol” at 80 mg twice daily could be used on any patient.
Evidence of abysmal treatment and lack of “supportive therapy”:
TEN patients mimic “Burn” patients in many ways because of the loss of skin although unlike the “Burn” patients, only the uppermost layer of the skin (“epidermis”) is affected in TEN. This is why modern day medicine recommends treatment of TEN patients in a specialized “Burn Center”. With appropriate care in a suitable center, TEN patients usually make a complete recovery in a few weeks time. Published international studies with large cohorts of TEN patients have shown virtually no death of any young TEN patients. Treatment of TEN patients basically involves aggressive “supportive therapy” which includes strict maintenance of fluid/electrolyte/nutrition balance through IV fluids and stringent control of infection. This has been clearly written in all the medical textbooks and testified by renowned dermatologists from across the world (see below).
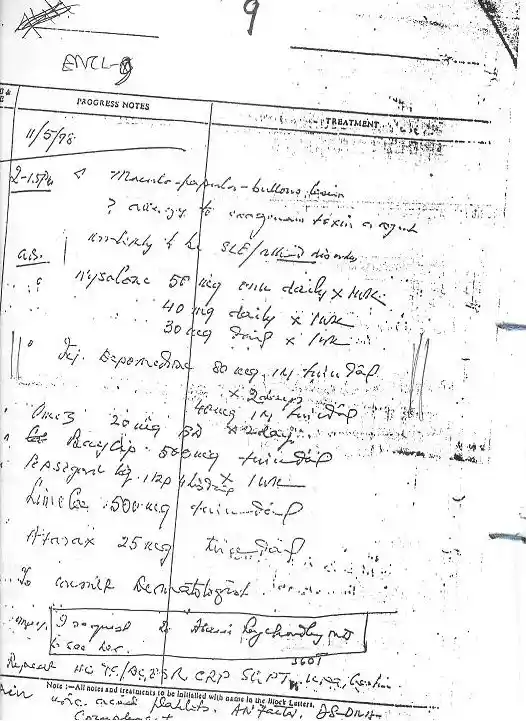
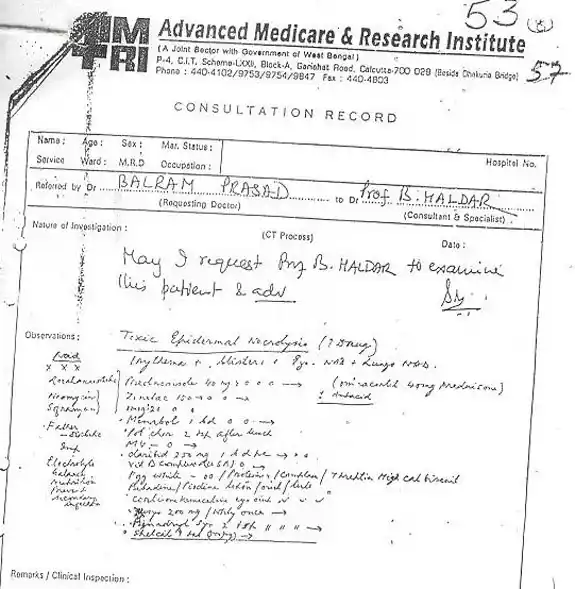
Anuradha was admitted in the AMRI Hospital in Calcutta on 11th May, 1998 in a serious condition at the advice of Dr. Sukumar Mukherjee. But after Dr. Mukherjee left for American later on the same day, Dr. B.N. Halder (Dermatologist) and Dr. Abani Roychowdhury (Medicine) jointly took over the charge for treatment of Anuradha (although after the criminal case was filed, Dr. Roychowdhury has claimed that he never knew or treated Anuradha). Dr. Halder first examined Anuradha on 12th May, 1998 and correctly diagnosed TEN. He also wrote a prescription (in consultation with Dr. Roychowdhury) which was basically followed during Anuradha's entire stay at the AMRI hospital. Although Dr. Halder stopped the long-acting “Depomedrol” which Anuradha had already received for the past 7 days at 80 mg twice daily dose, he added a different, albeit “quick-acting”, steroid (“Prednisolone”) without considering the devastating residual effect “Depomedrol” which was already pumped into the body of Anuradha. More importantly, Dr. Halder did not advise any of the mandatory treatment, i.e. “supportive therapy” which is essential for TEN patients. There were absolutely no specific instructions Dr. Halder/Dr. Roychowdhury for any IV fluid administration, care of the skin wounds or monitoring for any developing infection (through regular blood and swab tests) which are crucial for proper care of TEN patients. In fact, Dr. Halder and Dr. Roychowdhury advised not to “prick any needle” to Anuradha (with an obsolete and baseless fear that needle pricking might introduce infection) thus, totally ruling out possibility of administration of any IV fluids or blood tests. The hand-written prescription of Dr. Halder as present in AMRI hospital record is (shown in the next page) is a glaring example of gross medical negligence. First, Dr. Halder has not recorded a single clinical feature (e.g. pulse, respiration, physical description etc.) of the patient. Anuradha was very sick at this stage with large portion of her skin becoming loose or peeled off resulting in the loss of tremendous amount of body fluids through the denuded skin surface like in a “burn” patient. And there was absolutely no specific direction for replacement of the lost body fluid or monitoring of evolving infection. In fact, this same mode of therapy was basically followed for Anuradha until she became completely moribund and was shifted to the Breach Candy Hospital in Mumbai on 17th May, 1998.
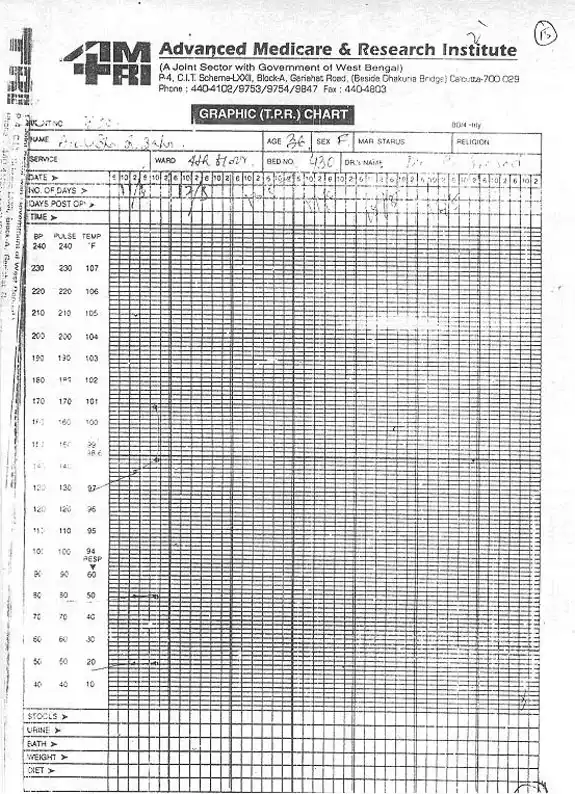
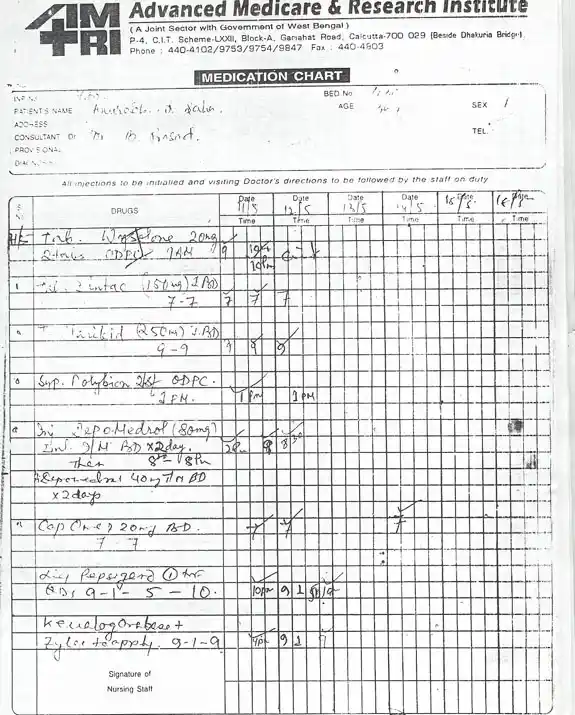
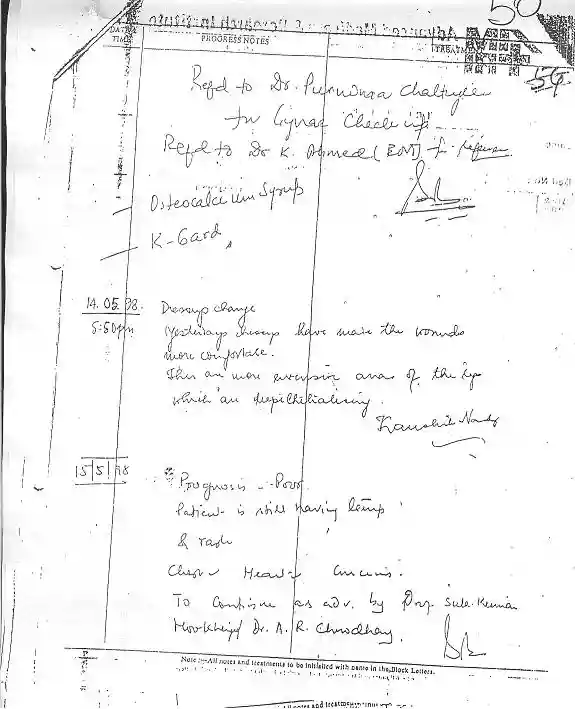
The rash and grossly negligent mode of Anuradha’s treatment at the AMRI hospital would be evidently clear from the hospital record itself. For example, despite being in an extremely critical condition going from bad to worse everyday, Anuradha’s minimal clinical parameters, such as “temperature”, blood pressure (b.p.), pulse/respiration rate and intake-output etc. were not measured at all after the first couple of days. As seen in the hospital temperatue/pulse/respiration (TPR) chart on the next page, Anuradha’s temperature was recorded only on 11th May, 2005 and despite a recorded temperature of about 1010F on 11th May, no further recording of her temperature was done until she left AMRI hospital. The b.p. and respiration rate were also recorded only on 11th May and the rest of the chart is completely blank. Even her “Medication Chart” shows (on page 28) that the drugs were given in a regular manner only on 11th and 12th May and only once on 14th May. No drug was given either on 13th May or anytime after 14th May even though Anuradha was treated at the AMRI hospital until the afternoon of 17th May when she was shifted to the Breach Candy Hospital at the advise of the senior dermatologist, Dr. B.N. Halder. This shocking hospital record glaringly underscores the pitiful status of the treatment given to Anuradha at the AMRI hospital. It is noteworthy that on 15th May, 1998, the resident physician at AMRI hospital has noted “Prognosis poor” (see page 29) but even after such dire comments by the attending physician, even the minimal care of the patient such as to check fever (temperature), respiration/pulse rate and b.p. was conspicuously absent at the AMRI hospital. Medical experts from around the world including Prof. Peter Fritsch from Austria, Prof. J.C. Roujeau from France, Prof. Gerald Pierard from Belgium and Prof. David Fine from USA who have evaluated Anuradha's treatment and AMRI hospital record have expressed their shock and disbelief at this mode of therapy and left no doubt that Anuradha was a victim of gross medical negligence (see their opinions below). There can be no dispute that the AMRI hospital record of Anuradha's treatment portrays an example of gross medical negligence of the worst kind. It may be pertinent to mention in this context that in the same note by the AMRI doctor on 15th May, 1998 (page 29), he has also mentioned, “To continue (treatment) as advised by Prof. Sukumar Mukherjee and Dr. A. Roychowdhury (Abani Roychowdhury)”, obviously suggesting that Anuradha's treatment was being followed at the advice of these senior doctors and it should continue in the same way. It is shocking that despite such irrefutable evidence present in the AMRI hospital record, Dr. A. Roychowdhury has pleaded in defense in the “criminal” case that he never treated Anuradha and did not even know her until the case was filed against him. As mentioned before, Dr. B.N. Halder issued a certificate on 16th May, 1998 urging to shift Anuradha to the Breach Candy Hospital where she eventually died.
Opinions from world-renowned medical experts:
Apart from the brazen and obvious evidence of gross negligence in the treatment of Anuradha as discussed above, Anuradha’s husband approached to many top medical experts (who are famous for their work on TEN). These experts include not experts not only from USA but also from France (Prof. J.C. Roujeau), Austria (Prof. Peter Fritsch), Belgium (Prof. Gerald Pierard) and even India (Dr. J.S. Pasricha, discussed above). All these experts have evaluated the treatment that Anuradha received in India and left no doubt that Anuradha died as a result of gross medical negligence. These experts’ opinions have been submitted in the court. It must be mentioned that while Anuradha’s husband has provided numerous experts’ opinions from around the globe showing that rash and negligent treatment was the reason for his wife’s untimely demise, none of the accused doctors could provide a single expert’s opinion, either from India or anywhere else in the world, in their support. Some of the international experts’ opinions about Anuradha’s treatment that were provided by the prosecution in this case are discussed below:
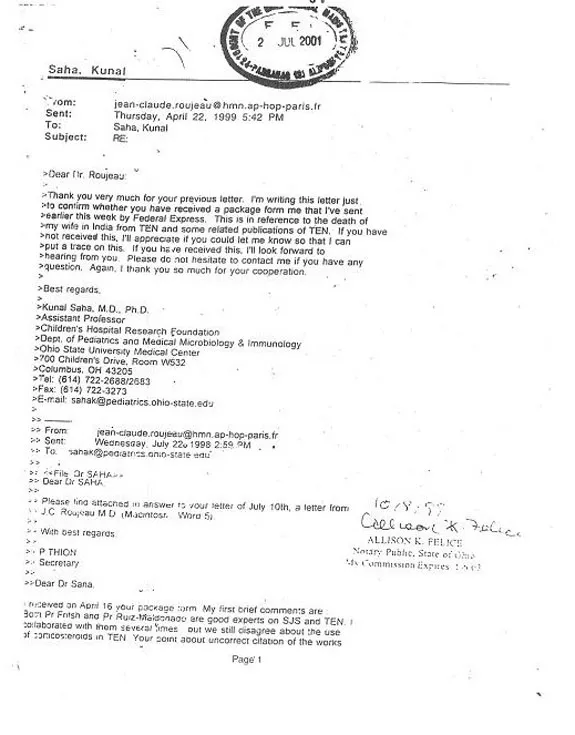
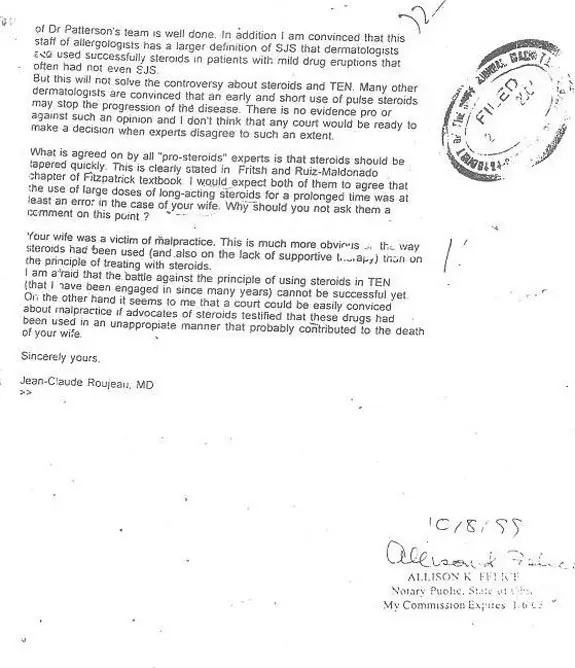
1. Prof. J.C. Roujeau from France (see page 33-34):
Prof. Roujeau is probably the most well-known TEN expert in the world who has published the highest number of scientific articles and major textbooks on TEN. While there is an absolute agreement about the aggressive use of “supportive therapy” for TEN patients, there is still some controversy whether or not any steroid should be used in TEN. While recent studies have shown that steroids have absolutely no beneficial effect in TEN and could be detrimental, some doctors still use steroids but only in the very early stage of TEN. Although Prof. Roujeau does not recommend any “steroid” for treatment of TEN like most medical experts in the modern time, he has acknowledged the existing controversy about steroid use in TEN and analyzed the obvious failure in Anuradha’s treatment considering the total perspective. In communication with Anuradha’s husband, Prof. Roujeau has clearly explained that Anuradha’s death has nothing to do with the controversy of steroid use in TEN and that even the pro-steroids experts should agree that her treatment was wrong not only for the inappropriate way that steroids were used but also for the complete lack of any “supportive therapy”. Prof. Roujeau has unequivocally stated to Anuradha’s husband, “Your wife was a victim of malpractice. This is much more obvious in the way steroids had been used (and also on the lack of supportive therapy) than on the principle of treating with steroids” (see page 34).
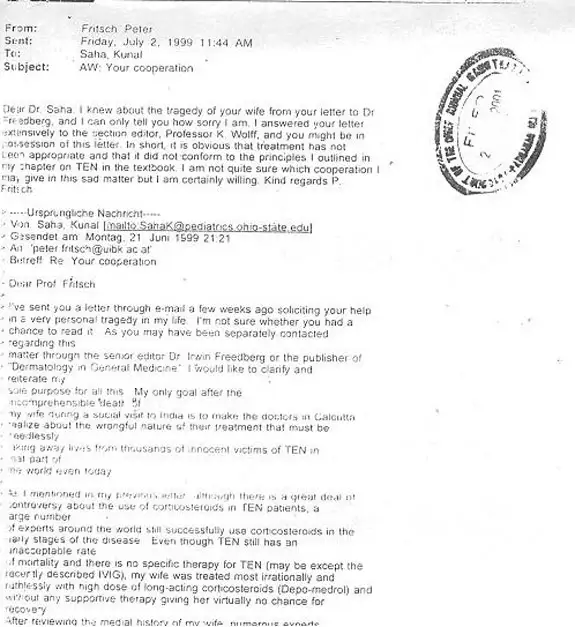
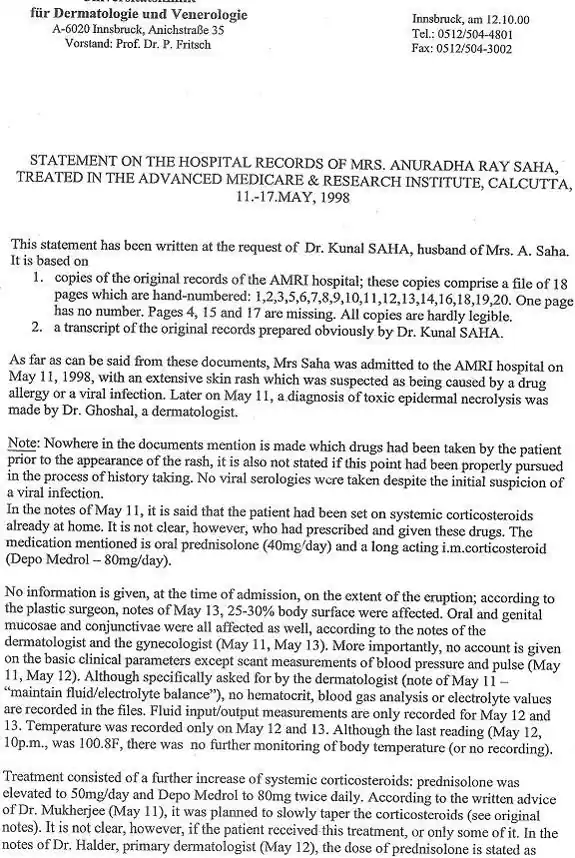
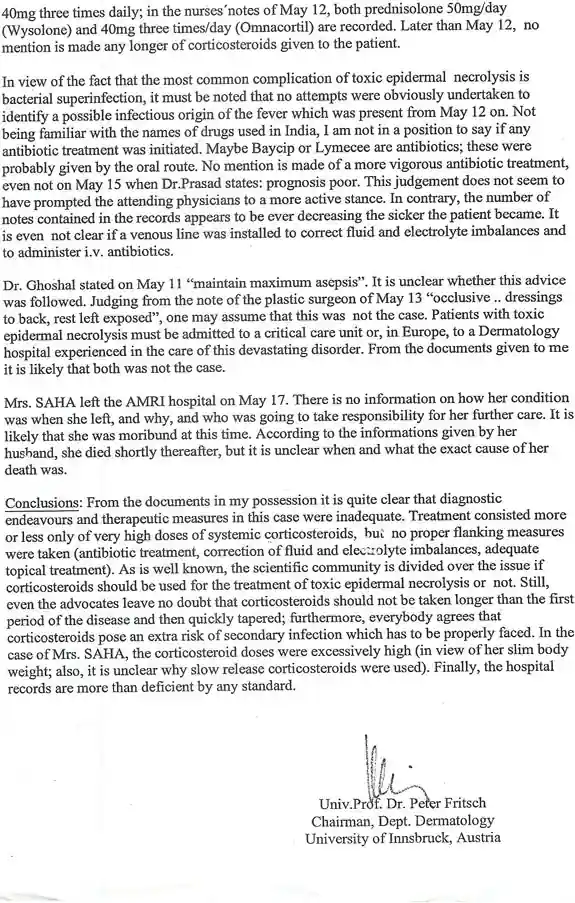
2. Prof. Peter Fritsch from Austria (see page 35-37):
Prof. Fritsch is also a highly respected TEN expert and the author of the chapter on TEN in the well-known dermatology textbook “Dermatology in General Medicine”. In fact, the accused doctors including dermatologist Dr. B.N. Halder claimed that they actually tried to follow Anuradha’s treatment as advised by Prof. Fritsch in this textbook only because unlike most expert in the West, Prof. Fritsch is “pro-steroid” and he still prefers to use some steroids in the early stages of TEN in a judicial manner. In email communication with Anuradha’s husband, Prof. Fritsch has categorically stated, “It is obvious that (Anuradha’s) treatment has not been appropriate and that it did not conform to the principles that I outlined in my chapter on TEN in the textbook” (see page 35). Prof. Fritsch has also made a detail analysis of Anuradha’s treatment from the AMRI hospital record and found glaring flaws in the treatment as he has observed, “No hematocrit, blood gas analysis or electrolyte values are recorded in the files. Fluid input/output measurements are only recorded for May 12 and 13. Temperature was recorded only on May 12 and 13. Although the last reading (May 12, 10 pm, was 100.80F, there was no further monitoring of body temperature……….In view of the fact that the most common complication of TEN is bacterial supreinfection, it must be noted that no attempts were obviously undertaken to identify a possible infectious origin of the fever with was present from May 12 on…….No mention is made of a more vigorous antibiotic treatment, even not on May 15 when Dr. Prasad states: prognosis poor. This judgment does not seem to have prompted the attending physicians to a more active stance. In contrary, the number of notes contained in the records appears to be ever decreasing the sicker the patient became. It is not even clear if a venous line was installed to correct fluid and electrolyte imbalances and to administer IV antibiotics”.
In “Conclusions”, Prof. Fritsch has categorically noted “…It is quite clear that diagnostic endeavours and therapeutic measures in this case were inadequate. Treatment consisted more or less only of very high doses of systemic corticosteroids, but no proper flanking measures were taken (antibiotic treatment, correction of fluid and electrolyte imbalances, adequate topical treatment). As is well-known, the scientific community is divided over the issue if corticosteroids should be used for the treatment of TEN or not. Still, even the advocates (of steroids) leave no doubt that corticosteroids should not be taken longer than the first period of the disease and then quickly tapered; furthermore, everybody agrees that corticosteroids pose an extra risk of secondary infection with has to be properly faced. In the case of Mrs. SAHA, the corticosteroid doses were excessively high (in view of her slim body weight; also, it is unclear why slow release corticosteroids (“Depomedrol”) were used). Finally, the hospital records are more than deficient by any standard” (see page 36-37)
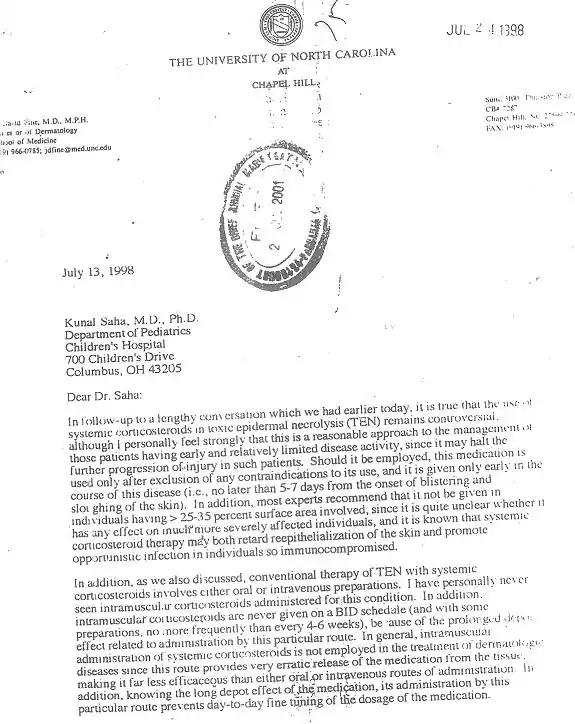
3. Prof. David Fine from USA (see page 38-40):
Prof. David Fine is a highly accomplished expert on TEN at the University of North Carolina and like Prof. Fritsch, he is also one of the rare dermatologists in the US who still prefer to use some steroids in the very early stage of TEN. Prof. Fine has also evaluated Anuradha’s treatment and provided his opinion as a “pro-steroid” TEN experts in a candid and elaborate fashion on two separate occasions, first on 13th July, 1998, soon after Anuradha’s death when her husband first contacted Prof. Fine for his opinion and next on 2nd October, 2000 expressing his intent to depose in this case, if necessary. As Prof. Fine has summarized in his letter (page 38), “The treatment provided to her (Anuradha) was clearly improper. Indeed, I would view this as gross malpractice based on the considerable medical literature on this subject, combined with my own personal experiences with this diseases over the past 22 years”. In his earlier letter in 1998, Prof. Fine made a thorough analysis about the use of steroids in Anuradha’s case and categorically stated, “Intramascular corticosteroids (“Depomedrol”) are never given on a BID (twice daily) schedule and with some preparations, no more frequently than every 4-6 weeks……..Although many authorities still use systemic corticosteroids in carefully selected patients with early TEN, the manner in which treatment was instituted in your wife certainly appears to be unprecedented” (see page 39-40)
Many other supporting experts’ opinions have been produced in the court in the “criminal” case for the wrongful death of Anuradha which are not shown here. In fact, apart from expert dermatologists, the prosecution also produced witnesses in the court during the criminal trial who were experts on “Pharmacology” (e.g. Prof. Salil Bhattacharya) and “Medicine” (Dr. A. Gupta and Dr. F. Udwadia). As mentioned before, Dr. J.S. Pasricha, eminent dermatologist from India also provided his opinion in this case in support of Anuradha’s husband, Dr. Kunal Saha. In sharp contrast, not a single expert’s opinion was produced by any of the accused doctors in support of their treatment of Anuradha either during the “criminal” trial or in the pending “civil” case for financial compensation.